This report outlines the progress made in 2024/25 by NHS England’s Healthcare Inequalities Improvement Programme (HIIP) and the NHS Race and Health Observatory (RHO) in identifying, measuring and reducing inequalities in healthcare access, experience and outcomes. It highlights how inequities by deprivation, ethnicity, and other social factors remain significant—but also shows how targeted programmes are being developed and embedded.
Key themes include:
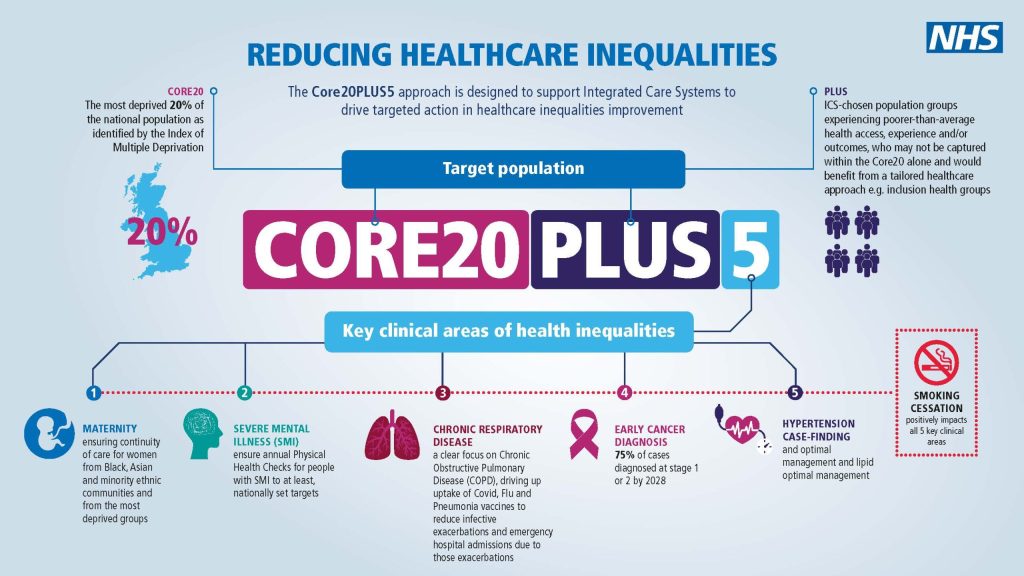
- Embedding the strategic framework using the “Core20PLUS5” approach (focusing on the 20% most deprived communities + inclusion health groups, with five clinical priority areas) across the healthcare system.
- Strengthening data, metrics and evidence: Developing new healthcare-inequalities metrics (e.g., adult and children’s programmes; ethnicity data) and embedding them in oversight dashboards.
- Implementation of targeted interventions: For example, improved support and digital care plans for people with sickle cell disorder; the launch of a translation/community-languages framework for people where English isn’t their first language; investment in place-based initiatives such as coastal navigator networks.
- Future direction and accountability: The report sets out strategic priorities for 2025-27—including the expanded role of the RHO in workforce equality (including race & protected characteristics) and embedding health-inequalities ambitions in the government 10-Year Health Plan.
Key Findings / Highlights
The RHO’s strategic role has been extended into the 2025-27 period, with a stronger focus on workforce equality and ensuring that equity is built into clinical guidance, workforce development and system-level change.
The HIIP has moved from planning into delivery: each frontline organisation now has a clear health-inequalities plan, and the system is beginning to collect measurable progress indicators.
Metrics for adult Core20PLUS5 priority clinical programmes have been agreed and will be tracked via the NHS England Performance Oversight Dashboard; children’s metrics are in progress.
A new framework on community-language translation and interpretation services was launched in June 2025, targeting people whose first language isn’t English.
Digital care plans for people living with sickle cell disorder have been rolled out, and gene-editing therapies are being made available for some rare conditions for the first time in Europe.
What is Core20PLUS5?
Core20PLUS5 is NHS England’s national approach to reducing healthcare inequalities.
It helps the NHS focus its efforts where they can make the biggest difference.
- Core20 – the 20% most deprived communities in England, identified using the national Index of Multiple Deprivation (IMD).
- PLUS – groups who experience poorer access, experience or outcomes, but who may not always live in the most deprived areas. This includes inclusion health groups such as people experiencing homelessness, asylum seekers, Gypsy, Roma and Traveller communities, people with learning disabilities, and others identified locally.
- 5 – five clinical priority areas where the NHS can have the greatest immediate impact on reducing inequalities:
- Maternity – reducing mortality and improving outcomes for mothers and babies
- Severe Mental Illness (SMI) – improving physical health and access to annual health checks
- Chronic Respiratory Disease – earlier diagnosis and better management
- Early Cancer Diagnosis – increasing uptake of screening and early detection
- Hypertension Case-Finding – improving identification and management of high blood pressure
Why it matters
Core20PLUS5 helps the NHS target its resources and efforts where health inequalities are greatest.
By focusing on specific communities and priority clinical areas, it supports more equitable access, better experiences and improved outcomes for groups who have historically been underserved.
Accessing the Report
The Full Report can be viewed HERE



Leave a Comment